|
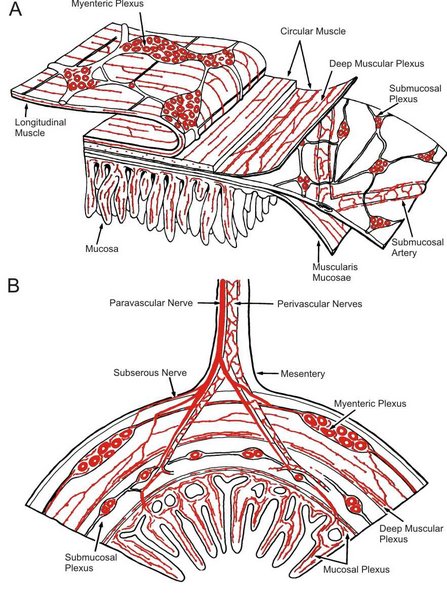
Within the gut wall there is a network of neuronal connections which senses chemical and physical changes in the gut lumen and in the gut wall, and causes reflex changes in the motility and secretion of the tissues. These local (intrinsic) reflexes include peristalsis. These enteric neurones communicate widely with each other and regulate digestive system activity.The intrinsic plexuses are located between the mucosa and the circular muscle (the submucosal plexus), and between the circular muscle and the longitudinal muscle (the myenteric plexus). The postganglionic neurones of the parasympathetic nervous system occur within the eneteric plexuses and behave as though they are the effector neurones for intrinsic reflexes, as well as the final effector neurones in the parasympathetic pathway. The parasymapthetic pathway tends to facilitate the activity of gut. Postganglionic neurones of the Sympathetic System terminate within the intramural ganglia, and generally inhibit the activity of intrinsic reflexes. |
|
|
Myenteric or Auerbach's plexus neurons innervate the muscle and secretory cells and contain different transmitters [acetylcholine, peptides like vasoactive intestinal peptide (VIP), substance P, enkephalin and nitric oxide or somatostatin]. These neurons may be excitatory or inhibitory - thiose containing nitric oxide synthase or somatostatin are generally inhibitory. Submucosal (or Meissner's plexus) contains the cell bodies of sensory fibers connected with sensory receptors deep in the mucosa and tranmits sensory information about mucosal conditions to the myenteric plexus. The arrangement of sensory and motor neurons within the gut wall allows for local or intrinsic nerve reflexes such as Peristalsis to occur. 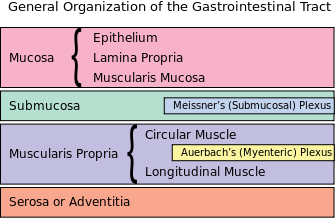
|
|
|
|
|
|
Peristalsis: a local reflex Peristalsis is a propagated wave of circular muscle contraction that moves down the intestine and propels intestinal contents on to the next segment of bowel. The smooth muscle ahead of the propagated contraction also relaxes. These events are mediated by intrinsic reflexes involving neurones within the gut wall plexuses. Sensory neurones respond to distension of the bowel, and these synapse on the neurones of the intrinsic plexuses, including effector neurones that release acetylcholine on the smooth muscle, causing it to contract. This final synapse in the pathway is sensitive to atropine, and is mediated by muscarinic receptors. | Segmentation Movements: generated by the spontaneous ativity of smooth muscle. Segmentation movements cause intestinal contents to be mixed, without being propelled down the gut. Segmentation movements are due to the spntaneous activity of smooth muscle; pacemaker cells and the interstitial cells of Cajal (ICC) may be involved in the genesis of segmentation movements. These movements can be speeded up by vagal stimulation, and suppressed by sympathetic stimulation.
|
|
The effector neurones of the intrinsic plexus behave as though they were the final post-ganglionic neurones of the parasympathetic supply to the GI tract. |
Chemoreceptors that sense the osmolality, pH, and presence of substrates and products of digestion are also present, particularly in the upper duodenum, and help to regulate gastric emptying and the secretions of the pancreas and gall bladder. |
|
The preganglionic fibres of the parasympathetic nervous system originate in the brain and in the sacral cord. These fibres release acetylcholine and excite the postganglionic neurones, a process mediated by nicotinic recpetors. The Vagus innervates the foregut, from the lower esophagus down to the transverse colon, whereas the parasympathetic supply to the lower gut is innervated from the pelvic nerves that originate in the sacral cord. | The postganglionic neurones of the sympathetic nervous system terminate on neurones of the intrinsic plexuses, and inhibit the reflex activities mediated by the plexus. Postganglionic sympathetic neurones also end on the blood vessels, as elsewhere in the body.
|