|
|
|
| The targets of the autonomic nervous system within the respiratory system are within the trachea and bronchial tree: bronchial smooth muscle and mucous glands (mucociliary clearance). Both influence the functional diameter of the airways, and therefore airways resistance. The upper thoracic sympathetic ganglia, and the dorsal motor nucleus of the vagus provide the autonomic nerves to the airways. | |
Airways Smooth Muscle The tone of bronchial muscle influences airway resistance, which is also affected by the state of the mucosa and activity of the glands in patients with asthma and bronchitis. Airway resistance can be measured indirectly by instruments that record the volume or flow of forced expiration. FEV1 is the forced expiratory volume in the first second of a forced expiration. The peak expiratory flow rate (PEFR) is the maximal flow (expressed as l/min) after a full inhalation; this is simpler to measure at the bedside than FEV1/FVC. PEFR and FEV1.0/FVC are affected by the diameter of the small airways, and the autonomic nervous system affects thee measurements largely because of changes in smooth muscle tone in the walls of these small airways. |
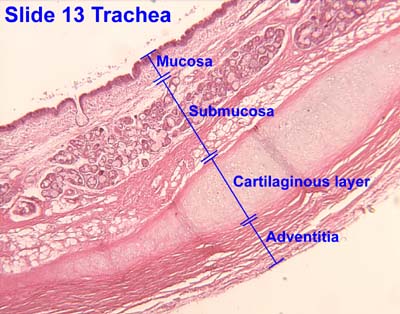
Respiratory Epithelium The respiratory epithelium consists of several cell types:
Basal cells appear to be precursors of other cell types, able to differentiate into them when repair of the epithelium is required. Beneath the muscosa are the submucosal glands that contain mucous cells and serous cells; the latter secrete fluids and ions and affect the thickness of the mucus in the airway. The Cystic fibrosis transmembrane conductance regulator (CFTR) is an ion channel that transports chloride ions across epithelia. Mutations of the CFTR gene affect functioning of the chloride ion channels in these cell membranes, leading to cystic fibrosis, which is characterised by the production of large amounts of thick mucous that accumulate in the bronchial tree and also in the pancreas. The sweat contains more salt than usual as a result of disruption of this ion channel. |
|
Mucociliary clearance The respiratory epithelium secretes mucus, which accumulates particulate inhaled matter, and this sticky mixture is moved up the airway system using the cilia of the respiratory tract ciliated epithelium. The thickness of the mucus depends on the amount of fluid secreted from the submucosal glands and goblet cells. Cilia normally operate in a thin film of mucus, and thicker mucus accumulates on top of this layer: this is where particulate matter and microbes stick. The cilia beat in such as way as to move the mucus towards the pharynx, thus removing it from the bronchial tree; it is normally removed from the pharynx by coughing. Failure of mucociliary clearance is associated with (a) thick mucus, and (b) failure of ciliary movement. |
|
|
|
|
Parasympathetic Nerves in the Airways. The parasympathetic ganglia are found in the bronchi and bronchioles, and innervate airway smooth muscle and glands. Acetylcholine is released from the postganglionic endings and acts on muscarinic cholinergic receptors in the target tissues. |
The parasympathetic innervation of bronchial smooth muscle is greater than that of the sympathetic system. Stimulation of the vagus causes bronchoconstriction, mainly within the larger airways. The vagus also causes secretion of mucus and this can be inhibited by stimulation of postganglionic sympathetic neurones, possibly because it reduces the blood supply to the glands by causing vasoconstriction. |
Sympathetic Nerves in the Airways Sympathetic nerves have a dense innervation of submucosal glands and blood vessels, but few are found in the airways smooth muscle in humans and mammals. The sympathetic innervation of respiratory tract glands causes secretion of fluids and mucus; alpha and beta adrenoceptors are present in these glands. β2-Adrenoceptors are, however, plentiful on human airways smooth muscle from the trachea right down to the small bronchioles. β2-Adrenoceptors are also found on mast cells, epithelium and submucosal glands and β-adrenergic agonists relax bronchial smooth muscle, inhibit mediator release from mast cells and increase mucociliary clearance. |
Second Messengers The cellular mediation of the parasympathetic effects involve an increase in cyclic GMP (cGMP), whereas stimulation of the sympathetic causes and increase in cAMP within the bronchial smooth muscle. The balance between levels of cGMP (parasympathetic) and cAMP (sympathetic) within these cells are important determinants of the diameter of the bronchi and bronchioles, and therefore airway resistance. |
|
Visceral Afferents Unmyelinated sensory fibres in the respiratory mucosa are excited by irritants -smoke and pollutants - inflammatory mediators and physical stimuli such as cold air. These sensory endings contain peptides such as Substance P, neurokinin A and neurokinin B (tachykinins). The tachykinins can be released using an axon (local) reflex, and act on smooth muscle, secretory, inflammatory cells and an increase in capillary permeability. This is known as neurogenic inflammation, and results in an increased thickness of the mucosa. Excitation of the irritant receptors, e.g. by smoke, causes reflex activation of the parasympathetic, resulting in bronchoconstriction and mucus secretion, and possibly an increase in mucociliary clearance; they also induce the cough reflex. |
Non-Adrenergic Non-Cholinergic (NANC) nerves Non-adrenergic non-cholinergic nerves in the respiratory tract are of two types: inhibitory and excitatory. Inhibitory NANC nerves can dilate bronchial smooth muscle because of the release of transmitters such as vasoactive intestinal peptide (VIP) and nitric oxide. Excitatory NANC nerves, can cause neurogenic inflammation, i.e mucus secretion, increased vascular permeability, vasodilatation and bronchospasm. There appears to be a complex interaction between these nerves and inflammatory cells, which is still being investigated. Some of these NANC nerves are afferent in nature, and release their transmitters when sensory endings are activated and action potentials are conducted along all the branches of the nerve endings (the axon reflex). |
|
|
|
|
Asthma is an inflammatory disease in which airways resitance is increased due to narrowing of the small airways. Narrowing of the airways can be due to
The FEV1.0/FVC ratio and the Peak Expiratory Flow Rate are used to monitor changes in airways resistance, and beta-2 agonists and muscarinic antagonists have important effects mediated by the autonomic nervous system.
| Adrenoceptors and Asthma Beta-2 adrenoceptor agonists remain the mainstay of treatment of asthma. Because of the high density of beta-2 adrenoceptors in the bronchi and bronchioles, these drugs cause relaxation of the bronchial smooth muscle. As a consequence they allow air to move in and out of the lungs more easily because of the dilated airways. Beta-2 agonists therefore increase the Forced Expiratory Volume and the ratio of FEV1.0 / FVC Muscarinic antagonists are also commonly used to counter the contractile effects of the parasympathetic nerves. Steroids are also used to reduce inflammation. Leukotriene antagonists are also useful in that they can antagonise the effects of certain inflammatory mediators. |