| Heart |
|
The Sympathetic Nerves to the heart originate from the first four thoracic segments of the spinal cord. They synapse in the sympathetic chain which at this level contains an enlarged ganglion called the stellate ganglion because it is star-shaped; it is also know as the inferior cardiac ganglion. The preganglionic fibres release acetylcholine which act on nicotinic synapses in the ganglia; the post-ganglionic fibres release noradrenaline. |
The postganglionic sympathetic fibres act on many structures in the heart, including
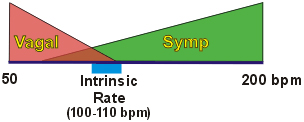
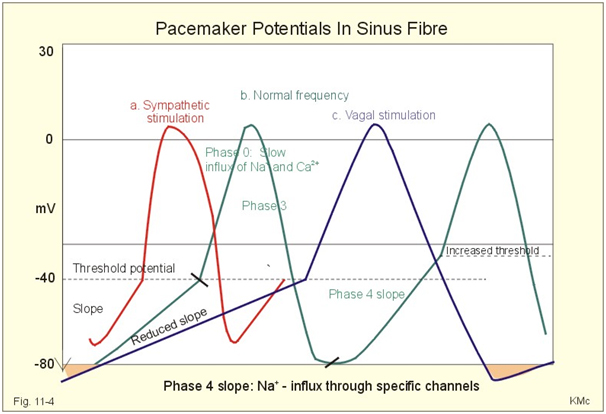
The sinu-atrial node (SA-node) is situated at the junction of the great veins and the right atrium. It is the site of origin of the spontaneous electrical activity (the pacemaker) that leads to the contraction of the heart. the denervated heart has an intrinsic rhythm of around 100 beats/minute, and this can be slowed or speeded up by the two divisions of the autonomic nervous system. The heart rate increases when the sympathetic nerves are stimulated because noradrenaline increases the rate of depolarisation in the S-A Node during diastole; these spontaneous depolarisations, known as pacemaker potentials, reach threshold more quickly as a result of the action of noradrenaline. The increased heart rate is known as Tachycardia. |
The parasympathetic nerves to the heart run in the vagus nerve. The preganglionic fibres originate from the dorsal motor nucleus of the vagus and synapse on parasympathetic ganglia within the heart. These, in turn release acetylcholine that acts on muscarinic receptors on the S-A Node, atrial muscle and AV-node. It has been thought that there are few vagal nerve endings in the ventricles, and that the effects of the vagus on the ventricles is insignificant. There are recent studies however that there is a significant affect of vagal postganglionic neurones on the ventricles, contradicting earlier assumptions. The frequency of the pacemaker is slowed during stimulation of the vagus nerve, and the slowing of the heart rate is known as Bradycardia. The rate of depolarisation of the pacemaker depolarisation is slowed during vagal stimulation, resulting in a longer period between beats (i.e. before threshold is reached). |
The diagram shows that the intrinsic heart rate generated at the S-A Node (~100/min) can be slowed by vagal stimulation (causing Bradycardia), and increased by sympathetic stimulation (causing Tachycardia). |
Cellular Basis for the actions of Sympathetic and Parasympathetic nerves on Heart Rate. The sinu-atrial node is the pacemaker and orgin of the heartbeat; it beats at the intrinsic rhythm of around 100 beat/minute. This is because the sinu-atrial node cells have a slow inward current which causes a pacemaker potential that brings the cells to threshold around 100 times per minute. The action of the vagus is to slow the pacemaker potential, so that it take longer to reach threshold; this results in a slowing of the pacemaker. Sympathetic nerves spped up the pacemaker potential, so that threshold is reached more quickly; this results in tachycardia.
|
|
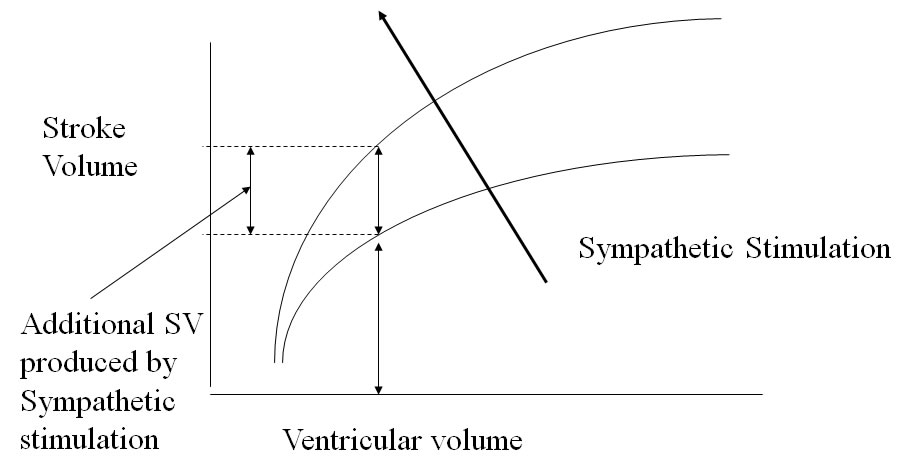
Actions of the autonomic nervous system on the contractile activity of the heart. Sympathetic nerves are present in the ventricles, and the release of noradrenaline causes the cardiac muscle to contract more strongly; the force of the contraction increases and therefore the power of the cardiac contraction is increased, and, if heart rate is unchanged, the cardiac output is increased. this is known as an inotropic effect, and is related to an increase in intracellular calcium concentration in the cardiac muscle. Positive Inotropism is present in the atria as well as the ventricles. The vagus nerve is often said to be distributed mainly to the atria, and to have only a small inhibitory effect on the force of contraction. Injections of molecules that act like acetylcholine however do reduce the force of the cardiac contraction, because there are muscarinic receptors in the ventricles. This is known as a negative inotropic effect. There is recent evidence that many (about one third) of parasympathetic postganglionic neurones contain nitric oxide synthase, an observation that can be made in other systems with autonomic innervation. This nitrergic innervation appears to have physiological effects on the ventricle and recent studies suggest that it appears to protect the ventricle agains ventricular fibrillation. |
Effects of sympathetic stimulation on stroke volume |
The Sympathetic Control of Blood Vessels. The vascular system consists of the pipes along which blood flows to and from the heart. The arteries take blood from the ventricles to the tissues The veins take blood back to the heart - from the tissues to the atria. Interposed between the arteries and veins there are many small tubes (arterioles, capillaries and venules). All blood vessels except the capillaries receive an innervation by post-ganglionic sympathetic nerves.. The sympathetic postganglionic nerves release noradrenaline close to the vascular smooth muscle cells. Noradrenaline acts on alpha-adrenoceptors at this site and causes contraction of the smooth muscle, and a consequent reduction in diameter of the vessel. In the arterioles this results in an increased resistance to blood flow - a means of regulating arterial pressure and altering the distribution of blood flow in the tissues. Contraction of venous smooth muscle makes the venous system less compliant, and causes a reduction in the capacity of the venous system and a rise in peripheral venous pressure. This mechanism is of some importance in haemorrhage, when the venous reservoir of blood can contract and ensure an adequate supply of blood to essential organs (e.g. heart and brain). |
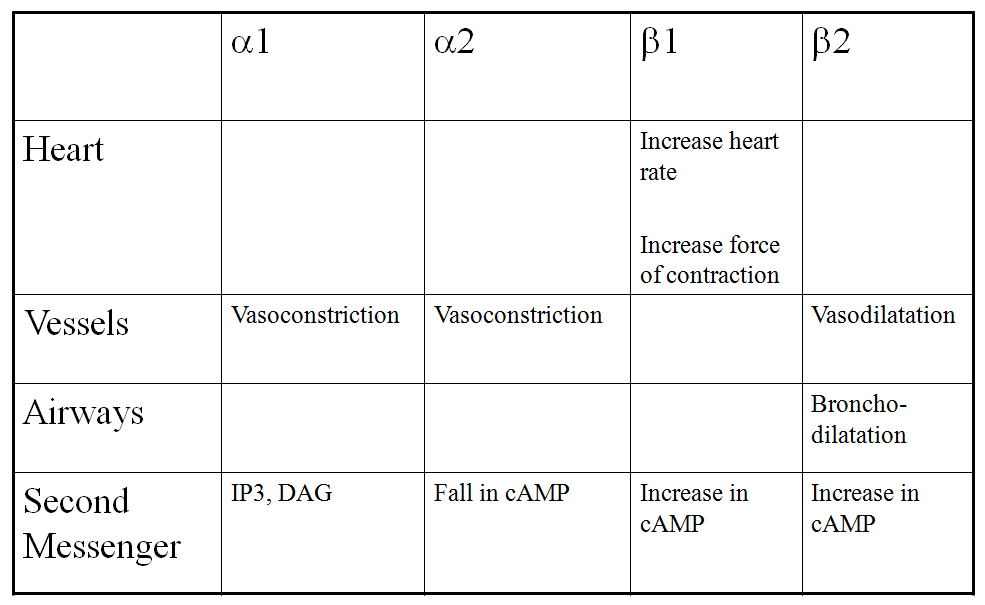
The major innervation of all blood vessels is through the sympathetic nervous system, which releases noradrenaline on to the vascular smooth muscle.. Noradrenaline causes vasoconstriction of arteries, arterioles, venules and veins, (in addition to tachycardia and a positive inotropic effect in the heart). The adrenoceptors are different however:
Adrenaline, released into the circulation from the adrenal medulla, has the same effects as noradrenaline on the heart, but has an additional vasodilator effect on blood vessels mediated by beta-adrenoceptors. The vasodilatation is seen when the concentrations of adrenaline are low, and at higher concentrarion the vasoconstriction mediated by alpha-adrenoceptors is dominant. Most blood vessels (arteries, arterioles, venules, veins) do not receive a parasympathetic supply. The exceptions are erectile tissue and the blood vessels in the brain. In erectile tissue the parasympathetic produces a powerful vasodilatation, which involves a subset of parasympathetic neurones that releasse nitric oxide.. In the brain, vasodilator effects of the parasympathetic are weak. Acetylcholine and drugs that mimic its action cause bradycardia and vasodilatation that is blocked by the muscarinic receptor antagonist, atropine. |
|
Second Messengers
Noradrenaline (sympathetic postganglionic neurotransmitter in the heart and blood vessels) causes vasoconstriction, tachycardia and a positive inotropic effect. In the heart it acts on beta-adrenoceptors, and in the vessels it acts mainly on alpha-adrenoceptors. The table opposite shows the second messenger systems involved.
|
|
|
Reflexes influencing the Sympathetic Nervous System Sympathetic Preganglionic Neurones receive some afferent inputs from nociceptors that enter the spinal dorsal horn. A consequence is that painful stimuli cause areterial pressure to increase. |
|
|
Central Control of the Autonomic Nervous System Autonomic Neurones in the cord receive powerful descending pathways from the brainstem and hypothalamus, which have an immense influence on the autonomic outflow. These influences include important reflexes originating from the arterial baroreceptors and chemoreceptors, and inputs from the limbic system, and will be discussed later |
|